UK medtech startup Acurable has gained FDA clearance for a novel wireless diagnostic device for remote detection of obstructive sleep apnea (OSA). A formal launch into the US market is slated to follow this summer. Its wearable is already being used by a number of hospitals in the UK (where it launched in 2021) and in the European Union, after obtaining local regulatory clearances in the region.
The startup, which was founded back in 2016, is the brainchild of Imperial College professor Esther Rodriguez-Villegas, director of the university’s Wearable Technologies Lab, who spent some 1.5 decades conducting research into using acoustic sensing for tracking respiratory biomarkers to diagnose cardiorespiratory conditions — work that underpins the commercial hardware.
The London-based startup raised an €11 million Series A round (~$11.8M) back in October with its eye on the US launch. Prior to that it received £1.8M (~$2.2M) in across three different grants from Innovate UK, a national body which supports product commercialization. Private investors in the medtech startup include Madrid-based Alma Mundi Ventures, London’s Kindred Capital and KHP Ventures, a healthcare-focused venture fund also in the UK which is a collaboration between two NHS Hospital Trusts (King’s College and Guy’s and St Thomas’) and King’s College London.
OSA refers to a chronic respiratory condition characterized by pauses in breathing caused by the person’s upper airway being obstructed during sleep. It’s thought to affect a small percentage of adults — around 1.5 million adults in the UK; and some 25M in the US (with many more people affected across the world) — and while not immediately life-threatening it can be linked to serious health implications since it can contribute to conditions such as cardiovascular disease, diabetes, dementia and even heart attacks, making treatment or management important.
Healthcare services often struggle to manage chronic conditions, given the expense of long term monitoring. But Rodriguez-Villegas explains that in the case of sleep apnea there is even a challenge for healthcare services to diagnose the condition — since traditional polysomnography tests are inconvenient and/or costly. (The patient is either asked to sleep overnight at a special center, where they’re fitted out with a bunch of wired sensors. Or else they are trained how to fit the various electrodes themselves at home, with the associated risk that the test will have to be repeated if sensors are incorrectly fitted or get detached during sleep.)
Acurable’s tiny, self-applied wearable has been designed to offer a far more patient-friendly (and cost effective way) for diagnosis of the condition — allowing for the testing to be both remote (in patients’ homes) and super simple so patients can self-administer it.
One early adopter of Acurable’s product — Dr Michael Harrison, a professor of surgery and pediatrics at the Children’s Hospital at UCSF — offers strong praise, writing in a supporting statement that the device has been “game-changing for our patients, as it is a much simpler and comfortable experience”, as well as talking up how it “enables clinicians to conduct multiple night studies at a time, improving patient outcomes by giving them a much speedier diagnosis”.
For her part, Rodriguez-Villegas says she saw a role for developing technologies to solve problems with a significant social impact by addressing healthcare bottlenecks associated with chronic (and often under-diagnosed) respiratory conditions, starting with sleep apnea. So the plan is for her startup to bring more wearables to market in future, for other respiratory conditions, such as COPD and asthma — all based on the core acoustic sensing IP developed for the first device.
“What I realised early on was that [chronic cardiorespiratory conditions] will not be something that could be solved if we continue with [traditional healthcare] processes — that it’s not a matter of pumping money into the system. Because there is also human resources. So you need the clinicians, the nurses, you need to understanding. So that’s where where my journey started with tech,” she tells TechCrunch. “Deciding how do we create techs that can solve the bottlenecks and make patients’ lives better?”
While core research underpinning the product has taken well over a decade, designing, prototyping and building the actual product took around six or seven years, according to Rodriguez-Villegas — so working on things like miniaturizing the hardware and designing a UX with high accessibility so it’s easy for patients of all ages (and tech abilities) to use which she says was a huge priority for her.
“The app is designed so that there is no room for a stress or failure,” she says, explaining how she pushed her design team to avoid assuming users would know how to navigate traditional software menu structures. “I had had to have lots of conversations with my UI people in the beginning because they couldn’t understand where it was coming from.”

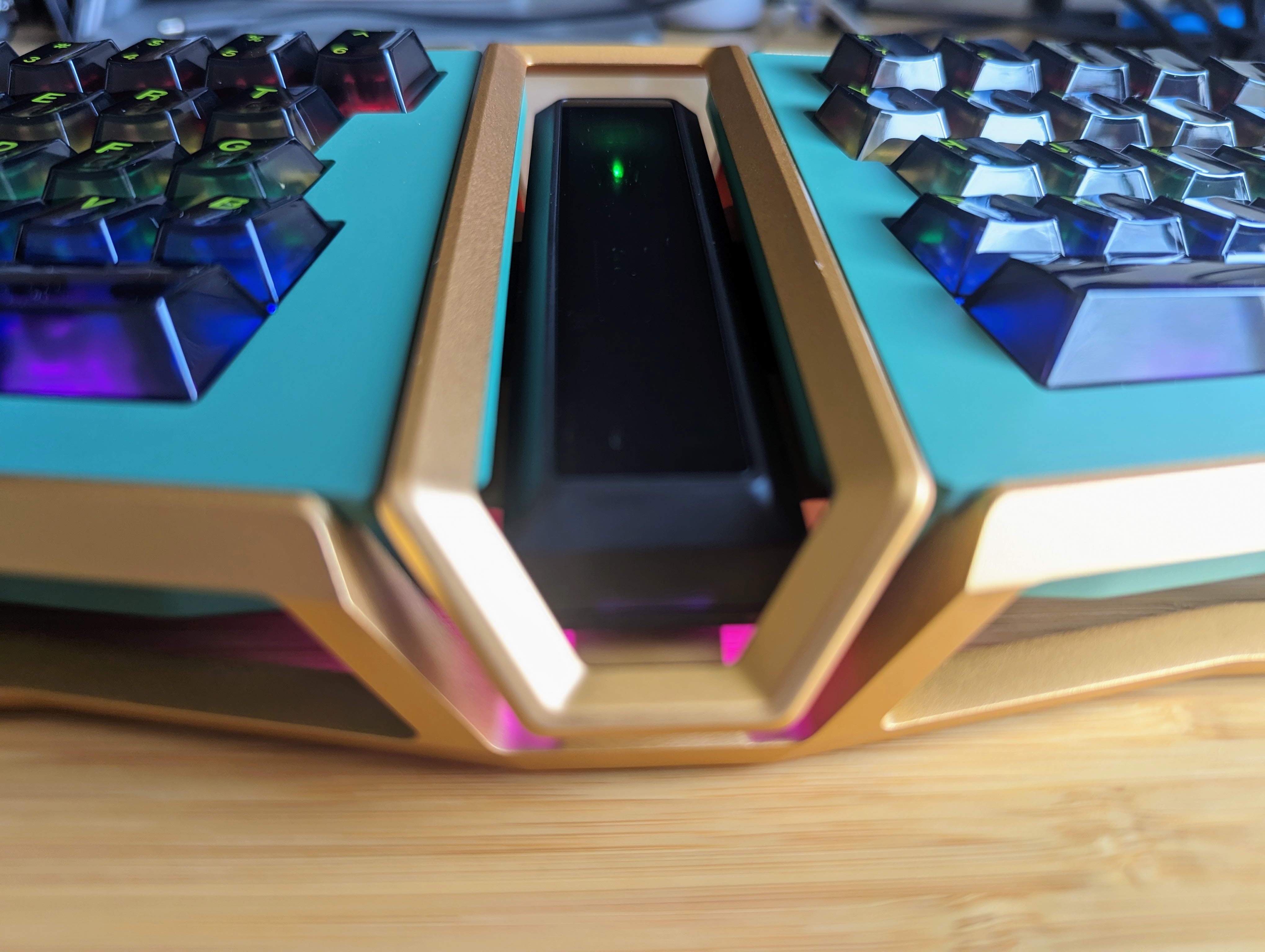
A patient self administering the AcuPebble with guidance from the app (Photo credit: Acurable)
As for the hardware, the startup’s one-shot sensing device, which is called the AcuPebble, looks a bit like a coffee pod that’s been colored an Apple-esque shade of shiny white. So sleek and minimalist looking is it that it resembles some kind of consumer device, rather than a medical instrument, with no utility grey plastic or scary bundles of cables in sight.
This purist look is entirely by design — reflecting Acurable’s overarching mission to rethink a convoluted diagnostic bottleneck using sensor-driven automation.
Patients use the AcuPebble at home where it’s worn overnight stuck to the the skin of their neck (using a patented adhesive). It’s also a single-use medical device — gathering and uploading enough data across one night’s tracking of the sleeper’s breathing to produce a diagnosis. (So to borrow another piece of Apple lore, you could say it’s designed to ‘just work’.)
The kit works by using tiny, high performance piezoelectric MEMS microphones to — in simple terms — listen to the patients breathing as they sleep. Although Rodriguez-Villegas is guarded with the exact details of how it works, saying the product is only partially patented so protecting IP remains a concern.
Acousing sensing as a diagnostic tool in healthcare is of course nothing new — just think of the stethoscope. But what’s novel here is the understanding of the sonic landscape associated with cardiorespiratory conditions that Acurable has been able to develop through years of research to isolate relevant biomarkers.
“The hardware is designed to detect particular biomarkers we are looking for and those biomarkers are very different to the conventional ones. And how do we know this? It’s again because it’s been almost two decades in the making,” says Rodriguez-Villegas.
The data the device captures is uploaded the cloud where it’s processed by Acurable whose algorithms produce an automated diagnosis which is sent to (human) clinicians for review. So much of the research which underpins the hardware was focused on understanding the specific ‘signal in the noise’ of the human body by winnowing down noisy human biology into the respiratory biomarkers of interest for diagnosing the particular cardiorespiratory conditions it’s focusing on.
The algorithms it’s using for diagnosis of sleep apnea are not machine learning or any other form of artificial intelligence. Nor is its approach data driven, per Rodriguez-Villegas, who emphasizes it’s using algorithms that are “fully traceable”. Although she does not entirely rule out using AI in the future — but is categorical that AI is unnecessary for this product and, indeed, that explainability in healthcare is an essential component; that there must be no black boxes for medical diagnostics.
“In this product — and the product in the market now — there is no AI. This is physiological signal processing based on very unique physiological modelling that we are experts on,” she says. “Everything in the algorithms happens for a known reason so the algorithms are fully traceable… Again, this is based on the research that we did in respiration for many years. That led us to that. It is not data driven. It’s really not data driven. I cannot really tell you exactly what it is. Because that’s part of the computational IP.
“But I do understand that everybody nowadays because AI is in everybody’s mind it’s almost like that is the default thought, right, that things are AI or they are data driven. No, no. We know why every single thing is happening. So in the same way, as you might know, you know, why your heart beats and [the steps in the cardiac cycle that take place around that] this is gonna be like that.”

Founder professor Esther Rodriguez-Villegas (Photo credit: Acurable)
Demonstrating the efficacy of its diagnostic algorithms was a core part of obtaining regulatory clearance for AcuPebble. And details of one clinical trial of the device, which was carried out at the Royal Free NHS Trust with a sample size of 150 patients — comparing usage to at-home multi-channel polygraphy followed by sleep specialist manual signal interpretation — can be found here.
Acurable says it was the first wearable medical device to obtain the CE mark in Europe for the automated testing of OSA at home. So, in its home region, it has regulatory clearance for fully automated diagnoses. But, in practice, the product has been set up so that the data (and diagnosis) are sent to a clinician — which helps keep these essential users comfortable with a novel tool — so there’s still a human in the loop.
Over in the US — where Acurable’s device will be officially launching at some point this summer — it’s obtained 512K clearance from the FDA for OSA evaluation in adults for two variants of the device customised for the American healthcare market. (Rodriguez-Villegas explains it did not file for de novo clearance since there is no existing device on the market that does automated diagnosis for OSA.)
The US versions of the product send data to a clinician to review and provide a diagnosis. So, in that market, it’s being strictly positioned as a clinical support tool. But that’s down to differences in the regulatory environment, rather than any technical difference in capability in the different per-market versions of the product.
It’s still early days for Acurable — with “tens” of hospitals using the AcuPebble at this stage. But it’s expecting usage to step up as it launches in the US and predicts it will be expanding its team by around 300%.
Rodriguez-Villegas also says it intends to expand into selling consumer products too “eventually” — but not before clinicians have been able to get comfortable with using the device and the data it provides.
She’s dismissive of current-gen consumer wearables — which can pack a range of health-tracking claims and even offer sleep apnea detection style features, such as by tracking nighttime SPO2 — saying a lot of these consumer wearables generate data that’s “very, very misleading” and creates “enormous amount of stress” for consumers. And indeed for the doctors faced with patients bringing in their own unreliable, non-medical grade health data.
“So that’s a situation that we totally want to avoid,” she adds. “Anyone can check our results. Is it is very, very good. It’s very, very reliable. But there is a lot of scepticism in the medical community when it comes to wearables. And that’s why we decided to go down [this regulated medical device] route.”
Meet the tiny, wireless sleep apnea diagnostic wearable headed for the US by Natasha Lomas originally published on TechCrunch








 English (US) ·
English (US) ·