One story from The Verge referred to Kindbody as the “SoulCycle” of fertility, pointing out that it sells fertility services and “empowerment” to 25-year-olds. It’s kind of a stretch, but I can see how the company could be compared to the aesthetic-driven facade of The Wing.
Kindbody isn’t solely selling a dream of belonging, however — there is a large focus on the consumerism of patient care. By concentrating on helping its patients feel like they have agency over their fertility journeys, Kindbody is trying to fit into the lives of those wanting to get pregnant.
“When you build businesses you have to think about how consumers behave today and what’s changed in the last five years or 10 years or 15 years,” Kindbody founder and chairwoman Gina Bartasi said. “And consumers crave and receive content.”
She recognizes how different the space is now compared to when she went through her own fertility journey.
“I think the hardest part is adapting, whether it’s adapting the media or adapting to healthcare,” she said. “You constantly have to have this circle and loop back with your customer and customer behavior and how that’s changed. And in healthcare, of course, your customer is the patient.”
Over the last decade, our lives have changed exponentially due to the easy access to information via social media platforms, and the COVID-19 pandemic only added a feeling of perpetual uncertainty. Businesses shut down for months at the top of 2020, schools have oscillated between mandating physical attendance and holding virtual classes nationwide, and offices that once forbade remote work have been introduced to hybrid setups like “hoteling.”
“The majority of patients need flexibility in their calendars,” Bartasi said. “I think, historically speaking, in health care, the patient did whatever the doctor did, whatever the doctor told them to do, and at Kindbody the patient is in charge, not necessarily the doctor.”
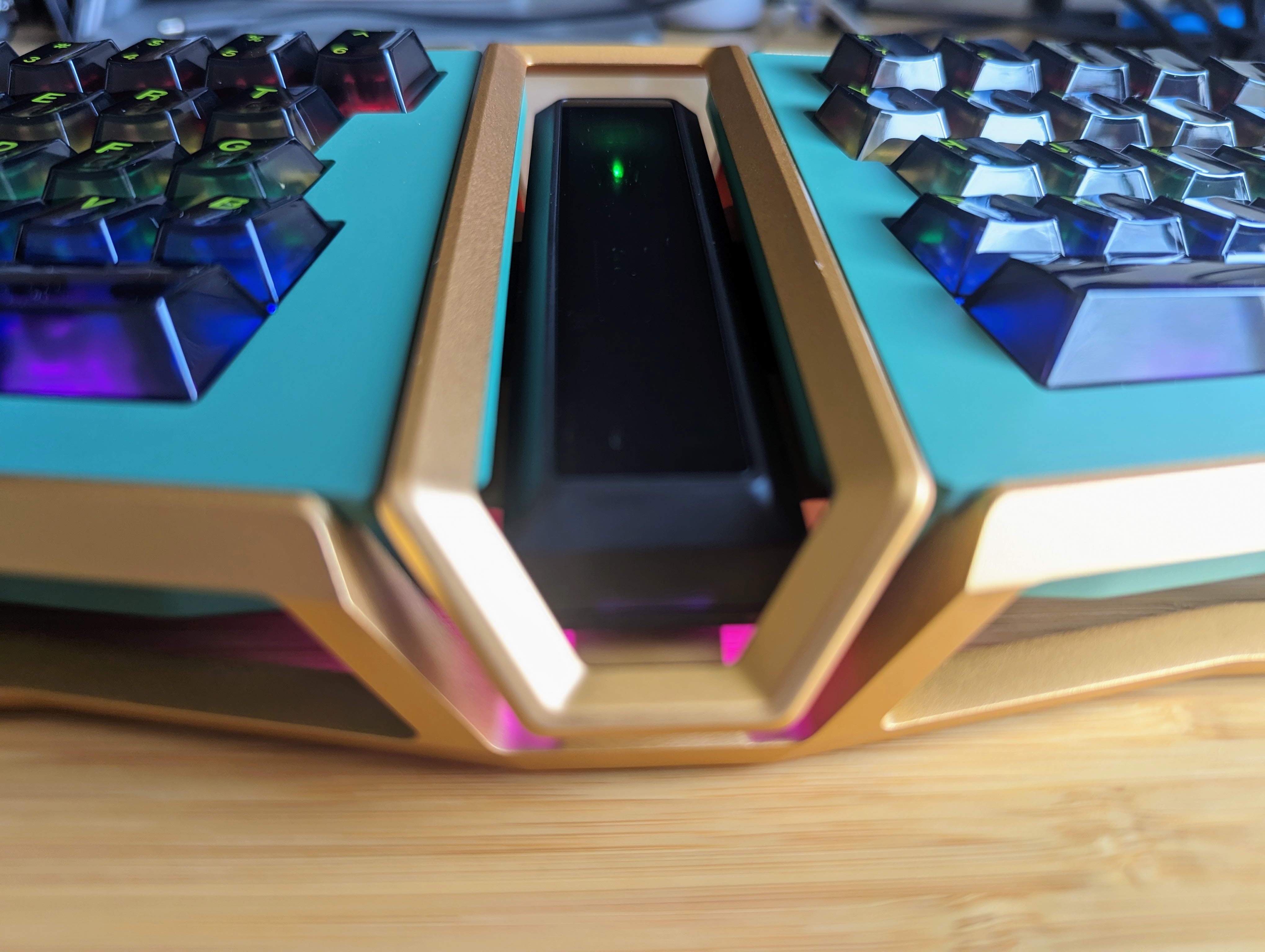
You can see this approach in nearly all of Kindbody’s services. Not only does Kindbody want to cater to how its potential patients carry on their lives, it wants them to have a familiar experience as well. Open Kindbody’s website, and you’ll find a templatized, user-friendly landing page with photos of well-designed offices and links to its social media. It’s a familiar look for the 2020s at this point, and that’s intentional.
With both B2B and B2C income streams, this company is trying to significantly disrupt the women’s healthcare space by focusing on educating, helping patients feel cared for and offering solutions to major pain points through employer-provided benefits.
As Bartasi mentioned in part 1 of this TC-1, she felt like she was treated as the subordinate to the doctor throughout her fertility journey, and her team at Kindbody has put in a lot of work to avoid that.
“It’s really a broken system”
Thanks to the nature of their relationships with the space, both Bartasi and Dr. Fahimeh Sasan, Kindbody’s current chief innovation officer and an experienced board-certified OBGYN, are familiar with the challenges of the fertility journey from two different perspectives — the patient and the provider. They found that the overarching challenge, which ultimately makes every step of this process more difficult, is the fragmentation of care.

Dr. Fahimeh Sasan, Kindbody’s chief innovation officer. Image Credits: Kindbody
“It’s really a broken system, and it’s a system that in no way, shape or form is based on proven human health nor on being proactive,” said Dr. Sasan. “It’s a 100% reactionary system. I was taught that you wait for a woman to prove that she’s not fertile and she has to prove her infertility diagnosis before you start doing testing and see if that’s what the problem may be.”
This reactionary approach is something she’s always felt needed to be corrected. She offers examples of how other ailments or potential health problems are addressed with the aim to prevent rather than cure.
“You do stress tests so that someone doesn’t have a heart attack. We do mammograms to detect breast changes before someone has breast cancer.” But when it comes to infertility, patients have to prove they are experiencing it before it can be addressed. She believes that the teaching and, subsequently, the care, have not caught up with the technology available for patients.
“If you think about the advancements that have been in this field, whether it’s the first egg-freezing or hormone-testing, like for the Anti-Müllerian hormone, and even the capabilities of ultrasound and sonogram, the teachings haven’t changed.”








 English (US) ·
English (US) ·